Articles & Product Documents, Clinical Journals
Minimally Invasive Techniques For the Private Practice Veterinarian: Laparoscopy and Video-Otoscopy
If you need to print this PDF or save for later
click below to download your copy.
Minimally Invasive Techniques For the Private Practice Veterinarian: Laparoscopy and Video-Otoscopy
Clarence A. Rawlings, DVM, PhD, Diplomate ACVS University of Georgia, Athens, Ga
Another reference is Small Animal Endoscopy, edited by Todd R. Tams and Clarence A. Rawlings and published December 2010 by Elsevier. The text, illustrations, and case studies are much more complete, as well as having a website that includes movies of cases and techniques.
A wide variety of diagnostic and treatment procedures are accomplished using rigid endoscopy. Diagnostic veterinary laparoscopy and thoracoscopy are used to view the surface of organs and to selectively biopsy focal lesions. Multiple biopsies of an organ, or of multiple organs, can be safely taken and the severity of hemorrhage assessed. One of the most valuable uses is to diagnose and stage abdomfnal cancer. Few veterinarians enjoy performing euthanasia of a favorite client’s pet when confirming by laparotomy that an abdominal mass is a non-operable cancer in a patient with relatively mild signs and a good quality of life. The rationale for intra-operative euthanasia is that the stress of recovery from a laparotomy exceeds the expected extension of a quality life. In contrast, two small incisions for laparoscopy are usually sufficient to confirm the same diagnosis and prognosis. The pet with mild clinical signs can then be recovered with much less stress. Diagnostic procedures remain commendable indications, but the greater impetus for laparoscopy has been the development of treatments traditionally reserved for open laparotomy..
Minimally invasive veterinary surgery reduces the surgical insult and would seem to be preferred over traditional open approaches. Reduced stress and small incisions have produced quicker recovery, decreased complications, and reduced infection rates. Although research studies have documented decreased stress responses following minimally invasive surgery, the primary motivation for endoscopy is that we would want laparoscopy and other minimally invasive surgery for ourselves as we believe it to be less invasive. Clients frequently rationalize, “I want the same advanced medical/surgical treatment for my four-legged family member as I want for myself.” The list of endoscopic treatments is long and continually expanding. We are selective on when to apply a procedure, based on the patient’s disease and the goals of the client. Whenever, endoscopy is used as the initial surgical technique, the client should be informed that conversion to a traditional laparotomy is an option if the surgeon determines that laparoscopy provides inadequate exposure to complete the procedure. We add to our informed consent form the statement, “…….Has permission to convert to a traditional (open) procedure if deemed necessary during endoscopic surgery.” Few procedures are converted, but the ability to do so enforces the client’s perception of the advantages of endoscopy, avoids potential intra-operative delay to convert, and increases the range of procedures than can be attempted knowing that there is minimal increase in risk to the patient.
Endoscopic Treatments
- Laparoscopic Incisional Gastropexy (Preventative and Treatment)
- Laparoscopic Enterostomy Tube Placement
- Laparoscopic Cyptorchid Castration
- Laparoscopic Ovarioectomy/Ovariohysterectomy
- Laparoscopic Cystopexy for Retroflexed Bladder in Penneal Hernia
- Laparoscopic Cystoscopic Calculi & Polyp Removal
- Laparoscopic Colopexy for Recurrent Rectal Prolapse
- Laparoscopic Gastrostomy for Foreign Body Removal
- Laparoscopic Attenutation of Portosystemic Shunts
- Laparoscopic Intestinal Resection and Anatomoses (& Enterotomy)
- Laparoscopic Cholecystectomy & Adrenalectomy
- Thoracoscopic Pericardial Resection for Pericardial Effusion
- Thoracoscopic Lung Lobectomy
- Thoracoscopic Connection of Persistent Right Arotic Arch & PDA
- Thoracoscopic Thoracic Duct Ligation for Chylothorax
- Transcervical Insemination
- Cystoscopic Resection of Ectopic Ureter
- Cystoscopic Resection of TCC
- Cystoscopic Injection Augmentation for Incontinence
- Rhinoscopic Resection of Nasal Cancer
- Otoscopic Debridement of Middle Ear Inflammatory Disease (Dogs & Cats)
- Endoscopic FB removal
Specialized endoscopy veterinary equipment includes surgical telescopes, camera, camera processing unit, a video capture or digital capture record to document images, monitor for viewing images, light source and cable, insufflation equipment to inflate the abdomen with carbon dioxide, suction, irrigation, and electrocautery. Electrocautery can be either monopolar or bipolar. Other energy sources include the harmonic scape!, “tissue sealing” bipolar electrocautery (LigaSure and Force Triad), and diode lasers. These provide hemostasis and dissection capabilities. Staples and vascular clips can be applied to individual vessels or be used to appose tissue. The light source and camera are attached to the telescope and insufflation line is connected to a side port on the trocar that is inserted into the abdomen. It is preferable to attach the insufflation line away from the telescope port to reduce fogging of the scope. Most telescopes are 5 or 10 mm in diameter, but arthoscopes can be as small as 1.9 mm. A 30 degree scope is used for “side-angled” viewing and a O degree scope for “straight-on” viewing.
Laparoscopy requires the abdomen to be distended with an optical media (carbon dioxide gas) in order to illuminate and view the abdomen. To prevent carbon dioxide from escaping, air-tight trocars are used as portals for the telescope and surgical instrumentation. Instruments are either 5 or 10 mm in diameter.
Biopsy coreneedles can be placed separately in similar fashion as whenperforming ultrasound directedbiopsies, anddonotrequirea trocaras their opening is small and does not permit gas leakage from the abdomen. A wide variety of terminal instrumentation can be passed through the trocars for dissection, tissue manipulation, ligation, vascular clip application, cautery, suturing, biopsy, and stapling.
Organ Biopsies and Cancer Staging Using Laparoscopy Assistance
Peri–operative Care
Pre-operative examinations for laparoscopic diagnosis are the same as for traditional surgeries. Evaluation of patients, selection of anesthesia, and peri-operative management is case based, with less consideration given to whether the procedure is performed by laparotomy or laparoscopy. Dogs with bleeding tendencies are poor candidates for surgery and coagulograms are commonly performed prior to any biopsy. The presence of decreased coagulation function or likelihood of poor healing following surgery is a strong justification for laparoscopy as compared to laparotomy. Much less tissue injury is produced during veterinary laparoscopy, thus reducing the potential for life threatening hemorrhage. Likewise, the decreased openings into the abdominal require less healing. Another strong indication for laparoscopy versus laparotomy is the presence of ascites, particularly that of a high-protein ascites. Biopsies can be obtained laparoscopically on most organs in the presence of ascites, leaving the ascetic fluid in the patient. When these ascetic animals are explored during traditional laparotomy this fluid and protein are removed. The patient will then have to replenish this abdominal fluid, resulting in a need for more fluid and protein, frequently by plasma and colloid administration.
Supportive care considerations are the same as for traditional anesthesia and surgery, except that the stress is usually less. Postoperative analgesia dosages may be lower than for traditional surgeries. Trocar sites can be blocked with bupivacaine in order to provide local analgesia. Most patients resume normal body functions, such as eating, defecating and early activity, more quickly than after traditional laparotomy.
Laparoscopy as a Diagnostic Tool
Nearly every abdominal organ or mass can be examined and biopsied laparoscopically. The two-dimensional image and ability to place the “seeing-end” of the laparoscope next to a mass produces vastly superior images to that seen by the naked eye during a laparotomy. Thirty-degree telescopes can be very useful to see around organs and masses. Gravity is the best retractor and is extremely useful during laparoscopy. Not only is gravity a better retractor than a mechanical spreader or assistant’s hands, this gravity is more gentle to tissues. By positioning the patient such that the area to be viewed is superior, the other organs move away and permit better examination. This is in contrast to the use of self-retaining retractors and assistant’s hands during traditional laparotomy, both of which produce trauma and can obstruct the surgeon’s view. Two senses are reduced during laparoscopy as compared to laparotomy. First, depth perception is reduced as compared to laparotomy. This reduced depth perception can be partially compensated by moving the laparoscope in and out. Second, direct digital palpation (feel) is not routinely performed during laparoscopy and feel is usually transmitted through endoscopic surgical instruments such as a palpation probe.
Liver Biopsies: Many patients with generalized liver disease and those with focal disease can be best sampled during laparoscopy. Biopsies are larger and have a much greater diagnostic accuracy than those obtained with 16 g or smaller core biopsy needles. In addition multiple biopsies can be taken with large biopsy cup forceps increasing diagnostic accuracy. Increased hemostasis can be provided by using mono polar electrocautery through the biopsy forceps or by adding Gel-Foam to the biopsy site. Cysts and the gall bladder can be aspirated using a 18G needle. When possible, it better to pass the needle through the quadrate lobe prior to entering the gall bladder. A spring-fired 14 g biopsy needle can be used to obtain samples from deep masses, but the biopsy cup forceps is nearly always used as the liver architecture can be better evaluated. The ability to examine the surface of the liver provides the opportunity to selectively sample focal lesions. Positioning the patient on their back with their head slightly elevated, rotating the body from left to right, manipulation of the liver, and the use of a 30-degree scope provide superior external examination of the liver. In contrast, a quick and usually adequate sampling of generalized liver disease can be done during heavy sedation, possibly supplemented with propofol with the animal in left lateral recumbency. Although much of the liver surface can be examined, it is more difficult to palpate the liver or to determine reasons for dilation of the biliary system. Seldom is much diagnostic information gained by palpation of the liver during a traditional laparotomy.
Kidney Biopsies: Biopsies of both kidneys can be safely obtained using laparoscopy. The diagnostic quality is greater than that performed with ultrasound guidance. There are a much greater number of glomeruli obtained when laparoscopy is performed with 14 g core biopsy needles. The ability to selectively biopsy the more superficial cortex increases the likelihood of obtaining good glomeruli samples and avoids arcuate vessels. In addition to avoiding arcuate vessels, additional hemostasis can be obtained by compression of the biopsy site with a laparoscopic instrument. Focal lesions can also be sampled.
Intestinal Biopsies: Full-thickness intestinal biopsies can be obtained. These biopsies can be multiple and selected from throughout the gastrointestinal tract. If only mucosa! biopsies of the stomach duodenum, or colon are needed, flexible endoscopy is preferred. To obtain full thickness intestinal biopsies, the intestine is lifted to the abdominal surface for a laparoscopic-assisted biopsy. The biopsy sites can protected following laparoscopic surgery by suturing either omentum or an adjacent jejunum to the sites. When jejuna! patches are used, care must be taken to insure that any jejuna! patch is separated at least 45 cm from the biopsy site, in order to reduce the likelihood that a stick foreign body can not travel through an acute intestinal bend.
Pancreatic Biopsies: Many internists and pathologists believe that too few pancreases have biopsies taken. A biopsy has been shown to be required to differentiate acute necrotizing from chronic pancreatitis in the cat, in contrast to clinical signs, enzymes, and ultrasonography. Pancreatic biopsies are taken by either a biopsy cup forceps or by using a endo-loop about a tip of the pancreas, and then cutting the biopsy from the distal portion.
Other Biopsies: Biopsies can be obtained from the prostate, spleen, lymph nodes and a wide variety of abdominal structures.
Laparoscopy as a Staging Tool
Laparoscopy can be a quick, low-stress method to obtain a histologic diagnosis and determine spread of an abdominal mass. In patients that can be identified as having a non-treatable cancer, it is frequently possible for the patient to recover from a minimally invasive evaluation and enjoy a short period of good quality life. It is usually possible to obtain a biopsy using two 5 mm trocars. One trocar is for a 5 mm laparoscope and the other a biopsy cup forceps. An alternative is to use the second 5 mm trocar to pass a manipulating instrument to aid in positioning abdominal contents in order to use a 14 gauge core biopsy needle. The best method of activating the biopsy needle is with a double spring-fired device. Multiple biopsies should be obtained from the primary tumor and samples should be taken from the lymph nodes most likely to provide lymphatic drainage. Some lymph nodes, such as the medial iliac lymph nodes are commonly used as sentinel nodes and should be routinely sampled in patients with perinea! and pelvic masses, or suspected prostatic cancer. Liver, spleen, and kidneys should always be examined in an attempt to identify tumors on their surface. Patients with effusions, especially when being present in both the pleural and the peritoneal cavities may be candidates for mesothelioma or carcinomatosis. Multiple biopsies should be taken from serosal surfaces. During laparoscopy, we attempt to leave the ascetic fluid in the patient to avoid producing a requirement for fluid and protein shifts.
If the mass appears to be potentially respectable and there is no evidence of obvious spread, laparoscopy can be converted to laparotomy for tumor resection. During laparotomy these masses may be resected, or additional information gained during the laparotomy may produce the diagnosis that the cancer will not benefit from surgery. We try to error on the side of conversion for masses deemed potentially respectable based on laparoscopy. Many of these decisions are also influenced by the patient’s overall health and the client’s desires for quality of life.
Laparoscopy for Surgical Treatments
At least a dozen laparoscopic treatments have been developed and are being used clinically in small animal practices. See list above. Minimally invasive surgery reduces the surgical insult and would seem to be preferred over traditional open approaches for any operation that can be performed by laparoscopy. Minimally invasive veterinary surgery treatments have dramatically advanced patient care for people; companion animal practice is following this trend. An excellent introductory technique is to use two 5 mm trocars for identification and extraction of an abdominal cryptorchid testicle through the trocar site for castration. The spermatic cord is ligated and returned to the abdomen. The same trocar site can be used to remove a second testicle if it is also retained.
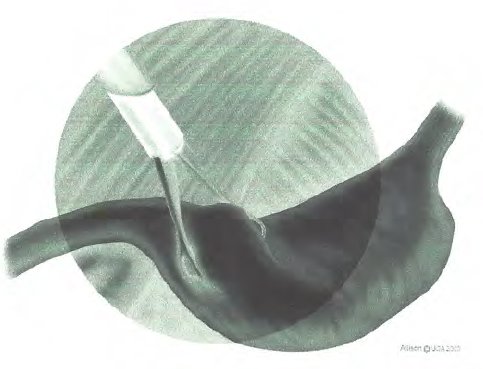
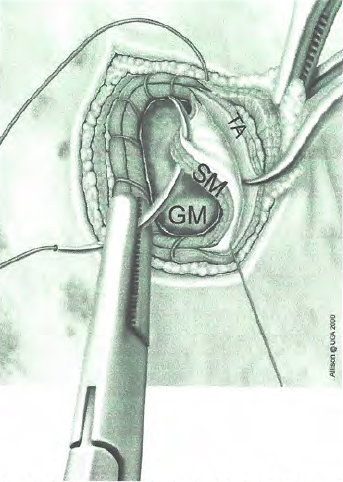
lncisional gastropexies are performed through one 10-12 mm trocar site and a second midline trocar for either a 5 or 10 mm laparoscope. (Fig. 2 and 3) This technique is strong, and easy to perform. The procedure was developed in research dogs and applied to a one-year prospective study of client-owned patients. Complications have been minimal; the gastropexy persists for a long time. Several hundred dogs have since been operated as well as many veterinarians being trained to perform the procedure. A trocar for insufflation and the laparoscope is placed on the midline, just caudal to the umbilicus. The second trocar is used for a 1O mm Babcock forceps and is placed lateral to the right edge of the rectus abdominus muscle and approximately 3 cm caudal to the last rib (Figure A). The antrum is lifted to the trocar site, which is lengthened sufficiently to perform an incisional gastropexy. The seromuscular layer of the antrum is sutured to the transverses abdominus (Figure B). Clients are urged to have an ultrasound examination performed within 6 to 12 months to insure that a gastropexy is present. Dogs with a gastropexy might bloat (gastric distention, only) and the appropriate treatment would be gastric decompression and fluid administration if volvulus is absent. In our prospective study, dogs had fewer gastric related signs after surgery than before gastropexy. Dogs with clinical signs of gastric dilation and volvulus also have been successfully treated laparoscopically.
Removal of cystic and urethral calculi using laparoscopic assistance to lift the bladder to the abdominal wall is very effective, reduces abdominal contamination with urine, and markedly improves ability to see the calculi and appearance of the bladder and urethra. Two trocars are used with the second site being enlarged just enough to lift the bladder to the abdominal wall. A mini-cystotomy is performed in order to place a 2.7 mm cystoscope. A variety of instruments are used to grasp and remove the calculi. The entire urethra can be examined to insure that all calculi are removed. To examined the male urethra, a 2.5 mm flexible scope is passed from the bladder antegrade into the urethra. This technique has been used to resect focal inflammatory polyps, to repair ruptured bladders, and to re-assess the sites of prior tumor resections. In similar laparoscopic-assisted fashion, foreign bodies have been removed from the stomach and intestines. Localized tumors and cecal-colic inversions have been resected with laparoscopic assistance.
Millions of ovariohysterectomies have been performed using traditional techniques in a similar fashion performed by James Harriot in the 1930’s. Recently, several laparoscopic and laparoscopic-assisted techniques have been developed to spay dogs and cats. Some studies have demonstrated that the stress response is reduced when the spay is done laparoscopically as compared to traditional surgery. I have recommended laparoscopic spays when other procedures (such as gastropexy) are being performed at the same time, in very large dogs, dogs with healing and coagulation deficits, and in dogs with residual ovaries. Other practitioners are routinely recommending that elective spays be performed routinely by laparoscopy. These include both ovariohysterectomies and ovariectomies. The latter is the standard procedure on the European continent and has been performed for decades with apparently no more problems that the traditional American ovariohysterectomy technique.
VIDEO-OTOSCOPY
Ear diseases are among the most common problems presented to the veterinarian. Dermatologists use the ear as a sentinel for generalized skin diseases, e.g. dietary based allergic dermatitis. Video-otoscopy is a vast improvement over traditional otoscopy as a diagnostic tool. The veterinarian can markedly improve your examination of the ear and equally important, the client can see and gain appreciation of the disease process. Practitioners using video otoscope daily strongly believe that client compliance is improved and that patients receive better ear care.
Ear Diagnostic Studies and Cleaning
Most ear diseases in dogs and cats are otitis externa, but otitis media must be rured out if topical treatment is to effectively treat otitis externa. Acute signs of otitis externa include hyperemia, edema, and excoriation. Chronic disease can lead to hyperplasia and even mineralization of the ear canal. Most patients have an abundance of smelly discharge and pruritus, as evidenced by head-shaking and pain. It is essential that a thorough dermatologic examination be done and the ear cleaned as the first step to ear treatment. Neurologic and otoscopic examinations are needed to rule out otitis media.
An ear swab for cystologic examination should be taken before ear cleaning. Cultures are commonly obtained. The exam should look for ear mites, foreign bodies, tumors, and character of the ear canal and tympanic member. Masses require either cytologic examination (fine needle aspirate, imprints of biopsies) or histopathology of biopsies. The cause of ear diseases can include infections (bacteria, yeast, fungi, viral, mites), foreign bodies (foxtail, plant, exudate), allergy (atopy, food, contact), endocrinopathies (hypothyroidism, sex hormone imbalances), seborrhea (primary, secondary), conformation (stenotic, hairy, polyps), immune mediated (pemphigus, lupus), and neoplasia (ceruminous gland T, squamous CC). Failure as a dermatologist frequently results in inappropriate or non-compliant treatment, e.g. failure of medical treatment and a need for surgery.
Since most ear dermatologic conditions have a secondary bacterial component and an allergic (or at least an excessive inflammatory) response, both antibiotics and corticosteroids are used topically. Antibiotics are given systemically when the middle ear is affected and systemic corticosteroids (anti-inflammatory dosage of 0.5 mg/kg for 5-10 days) are frequently needed to reduce inflammation. Fungal and mite infections require specific treatment. In general dry ears would require oily vehicles, but most are moist and exudative, thus requiring water-soluble vehicles. Eye medications may be used in the ear. All agents intended to treat specific agents must be administered to ears that have been just cleaned of debris if treatment is to be successful.
The most common explanation for treatment failure is to blame the client for not being compliant, but that may not be fair. Exudate must be removed initially by the veterinarian and then regularly before each treatment. Exudative processes may not be arrested and persistently insulate organisms from drugs. Conformational problems of pendulous ear pinnae and hairy canals and excessive moisture (swimming and pendulous ear canal) result in some breeds being very susceptible to ear disease.
Ear Diagnostic Studies and Cleaning
Indications to do a video otoscope are: 1. Owner’s comment about signs of ear disease, 2. Ear odor, discharge, or pain, 3. Older dogs undergoing a geriatric exam, 4. Breeds commonly effected by ear disease, and 5. Chronic skin disease. Video-otoscopy done in the outpatient room is typically done in the examination room with an awake or sedated patient. This is a cursory exam at the best and should be restricted to evaluating a healthy ear with no clinical signs. If the ear is found to be inflamed, painful, full of purelent material, etc. anesthesia is required to perform an thorough and diagnostic examination. The combination of anesthesia, improved video images, and irrigation through the scope increases visualization of the ear canal and tympanic membrane. It is the best technique to determine is otitis media is present. Undiagnosed and managed middle ear disease is a common cause for persistent otitis externa. In addition, failure to rid the ear of exudate makes it nearly impossible for medication to have an effect.
Instrumentation for video-otoscopy includes the standard camera/light/image processor endoscopy tower for use with a video-otoscope cone and with small diameter endoscopes. These can be the 1.9 and 2.7 endoscopes with their cystoscope sheaths. The scopes have a 30 degree viewing angle and the sheaths have an operating channel. Arthroscope sheaths also work well and provide excellent avenue for irrigation. Ancillary equipment include biopsy forceps, foreign body removal forceps, curets, ear loops, mosquito forceps, alligator forceps, and suction.
Clinical experience have shown that video-otoscopy is an excellent approach to manage middle ear disease by lavage and cleansing of the middle ear via the ruptured tympanic membrane. The approach requires persistent treatment by the client and regular video-otoscopy re-examinations.
 .
. 
Recommended Reading
Cole TL, Center SA, Flood SN, et al: Diagnostic comparison of needle and wedge biopsy specimens of the liver in dogs and cats. J Am Vet Med Assoc 2002; 220: 1483- 1490.
Devitt, Chad M.; Cox, Ray E.; Hailey, Jim J: Duration, complications, stress, and pain of open ovariohysterectomy versus a simple method of laparoscopic-assisted ovariohysterectomy in dogs. Journal of the American Veterinary Medical Association 2005-09-15227:6, 921-927,
Evans SE, Bonczynski JJ, Broussard JD, et al: Comparison of endoscopic and full thickness biopsy specimens for diagnosis of inflammatory bowel disease and alimentary tract lymphoma in cats. J Am Vet Med Assoc 229: 1447-1450, 2006.
Freeman LJ, editor. Veterinary Endosurgery. St. Louis: Mosby, 1998. McCarthy TC, editor. Veterinary Endoscopy. Philadelphia: Saunders, 2004.
Goethem BV, Schaefers-Okkens A, Kirpensteijn J: Making a rational choice between ovariectomy and ovariohysterectomy in the dog: A discussion of the benefits of either technique. Veterinary Surgery. 2006: 35; 136.
Hancock RB, Lanz 01, Waldron DR, Duncan RB, Broadstone RV, Hendrix PK: Comparison of Postoperative Pain After Ovariohysterectomy by Harmonic Scalpel Assisted Laparoscopy Compared with Median Celiotomy and Ligation in Dogs. Vet Surg 2005: 34; 273.
Hernadez-Divers SJ, Rawlings CA: Rigid endoscopy in small and exotic animals. Vet
Med2003;98:640-643.
Rawlings CA, Foutz FL, Mahaffey MB, Howerth EW, Bement S, Canalis C: A rapid and strong laparoscopic-assisted gastropexy in dogs: Am J Vet Res. 62: 871-875, 2001.
Rawlings CA: Pearls of Veterinary Medicine: Laparoscopic Assisted Gastropexy. J Am Anim Hosp Assoc. 38: 15-19, 2002.
Rawlings CA, Howerth EW, Bement S, Canalis C: Laparoscopic-assisted enterostomy feeding tube placement and full-thickness biopsies with serosal patch in dogs. Am J Vet Res. 63: 1313-1319,2002.
Rawlings CA, Howerth EW, Mahaffey MB, Foutz TL, Bement S, Canalis C: Laparoscopic-assisted cystopexy in the dog. Am J Vet Res 63: 1226-1231, 2002.
Rawlings CA, Mahaffey MB, Bement S, Canalis C: Prospective evaluation of laparoscopic-assisted gastropexy in dogs susceptible to gastric dilatation. J Am Vet Med Assoc. 2002;221:1576-1581.
Rawlings CA, Barsanti JA, Mahaffey MB, Canalis C: Laparoscopic-assisted cystoscopy for removal of calculi in the dog. J Am Vet Med Assoc. 2003; 222: 759-761.
Rawlings CA, Diamond H, Howerth EW, Neuwirth L: Diagnostic quality of percutaneous kidney biopsies obtained with laparoscopy versus ultrasound guidance in dogs. J Am Vet Med Assoc. 2003; 223: 317-321.
Rawlings CA, Howerth EW: Obtaining Quality Biopsies of the Liver and Kidney. J Am Anim Hosp Assoc. 40: 352-358, 2004.
Saunders HM, Vanwinkle TJ, Drobatz Ket al: Ultrasonographic findings in cats with clinical, gross pathologic, and histologic evidence of acute pancreatic necrosis: 20 cases (1994- 2001). J Am Vet Med Assoc 2002; 221: 1724-1730.